My first episode of psychosis arose from a brutal depression. A verse began playing in my head — from a voice that was male, angry and loud. I would later learn that this was The Voice of my psychosis, returning each time my symptoms did. He chanted in a deep timbre and his lyrics took on a mesmerizing rhythm.
“You are the charmed one
You are evil incarnate
You will vanquish evil
You are invincible.”
This episode, and the series of psychotic episodes that followed, occurred in the 90s. However, it wasn’t until I started working with a psychiatrist, Dr. Lev, in 2005 that I disclosed my experience. When I began working with this doctor, I was in the midst of yet another episode of suicidal depression, and I endured six inpatient psychiatric admissions over 18 months. During this prolonged episode, the bouts of psychosis returned.
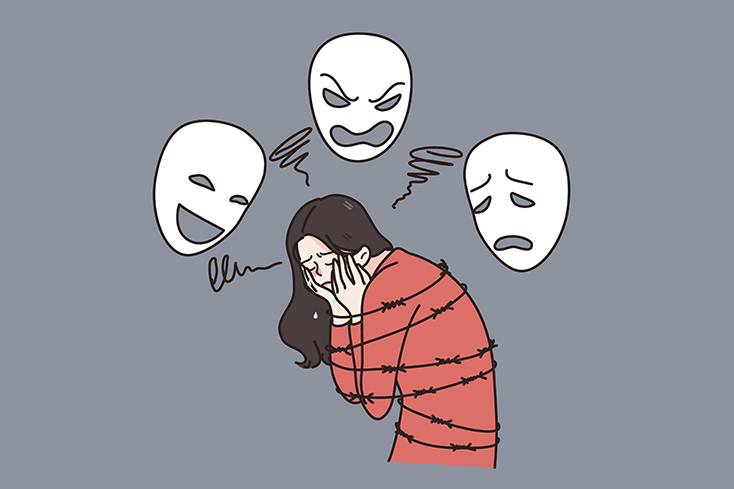
I needed to know I could trust Dr. Lev — that she would believe me, and she wouldn’t laugh at what I was revealing. My fears are not uncommon; people with mental health conditions are often hesitant to let others know they are experiencing psychosis.
As my experience suggests, addressing this symptom can be a challenging and isolating experience. However, learning to trust my doctor and working with her to find the right treatment plan has been key to my recovery.
Psychosis Left Me Feeling Ashamed And Scared
I often revisit my experience by reading files from my hospitalizations. An excerpt from an admission note to an inpatient treatment facility in September 2005 read, “patient describes hearing messages coming to her from the radio, somber music playing and commentary voices.”
When those of us who live with psychotic depression are experiencing delusions, we are often aware our thoughts are unreal, though there may be an element of doubt. This knowledge can feel terrifying as we wonder if we are gradually crossing the line from “sanity” to “insanity.”
In March of 2014, during one inpatient stay, a psychologist interviewing me inquired about psychosis, and I hesitated, falling silent and lowering my eyes. As I stared at the floor and played with my sleeve, I revealed to her that my room in the hospital was freezing, and I believed the maintenance men were following an unknown executive’s orders, purposefully blowing cold air through the vent up from the basement trying to freeze me out.
My Delusions Often Centered My Fear Of Abandonment
Each spring, Dr. Lev took a vacation to Europe for three weeks. Whenever she left for these trips, my mental health would deteriorate, and my intense fear of abandonment emerged. Each time, I became convinced she would choose not to return.
In 2010, the Icelandic volcano Eyjafjallajökul erupted, sending volcanic ash over nine kilometers into the sky. Europe experienced air travel chaos for almost one month. I became convinced that my desire to prevent my doctor from leaving was so strong, I’d caused the volcano in Iceland to erupt, preventing her from flying to Europe. Part of me knew I couldn’t possibly have triggered the volcano thousands of miles away. However, I feared that there was a fragment of my psyche that was conspiring against me. I could feel the gears grinding in the depths of my brain and The Voice rising to just under the surface taunting me:
“It’s all your fault.
You know you wanted this to happen.
You ought to be ashamed of yourself.
You’d better not tell.”
Eventually, I did confess my delusion to my doctor, and we explored the root cause of my fear of abandonment (and my enduring terror she would decide to permanently stay in Europe). In disclosing the delusion, I also feared The Voice would punish me for divulging our secret. I revealed to her if she didn’t return, I didn’t think I could survive without her.
Admitting how dependent I’d become on her made me feel as though I was a child begging a parent not to leave. However, she did not laugh or stop seeing me due to my attachment — she stuck with me and helped me find the medication regimen that kept The Voice at bay.
I Have Found An Effective Treatment And Continue To Make Progress
My regimen of psychotropic medication includes two antidepressants and one of the second-generation antipsychotics. I take these on an ongoing basis, not waiting for an episode of psychotic depression to occur first. Dr. Lev and I feel that it’s critical to be proactive due to my history and genetic predisposition.
It’s been almost a decade since I’ve suffered a severe depressive episode with psychotic features — a decade since I’ve heard The Voice — for which I am thankful. I’m also acutely aware for a person with my history, there are no guarantees. There seems to be no rhyme or reason to how my psyche functions — and even though I worked hard in therapy to gain insight into self-sabotaging patterns and behaviors, there is so much we don’t know about the brain.
There are days I feel the ground is solid beneath my feet, and there are days I feel the soil shifting and it’s as though the ground might swallow me into a world of unreality. Staying right side-up requires working hard every day, listening to my doctor, using the insights I gained in therapy and trusting my brain won’t betray me. Because life is still more of an art than a science.
Andrea Rosenhaft is a licensed clinical social worker in the New York City area. She is recovered from anorexia, major depression and borderline personality disorder (BPD). She writes and blogs on the topic of mental health and recovery. Andrea is also the founder of BWellBStrong, a mental health treatment consultation service organization which focuses its efforts on BPD, eating disorders, anxiety and major depressive disorder. She lives in Westchester, N.Y., with her rescue dog Shelby.
